Elevating Chiropractic Care to New Heights
Discover a fresh, clinically focused approach to pain management care in Mount Pleasant, SC—one that goes well beyond chiropractic adjustments.
A CLINIC YOU CAN TRUST
At The BodyFix, we provide far more than traditional chiropractic care. Every visit is customized to meet your specific needs, incorporating a range of advanced therapies and wellness modalities. Our goal is to address both your symptoms and their underlying causes, supporting whole-body health from the ground up. With a personalized treatment plan designed just for you, The BodyFix delivers comprehensive care to help you move, feel, and live your best.


DR. MARIO TOLJ
Owner/ Doctor of Chiropractic
Dr. Mario Tolj, founder and head clinician at The BodyFix Clinic, has been in practice for over a decade and brings a caring, patient-first mindset to every appointment. With extensive training in chiropractic care and a wide range of complementary therapies, he tailors each treatment plan to address the true source of discomfort and support long-term wellness. His whole-body approach, combined with a commitment to modern, effective techniques, has helped countless patients improve their movement, health, and overall quality of life.
OUR SERVICES
Every service we provide is personally recommended by Dr. Mario to ensure you receive the most effective, results-driven care.
Personalized, whole-body care:
Instead of one-size-fits-all adjustments, we tailor every treatment to your unique needs — targeting the root causes of pain or dysfunction rather than just masking symptoms.
Quality over quick “cracks”:
Sessions are 20–30 minutes — long enough to properly address muscles, fascia, ligaments, and joints — instead of rushing through a quick adjustment.
Comprehensive treatment tools & therapies:
We offer more than spinal manipulation: soft-tissue techniques, myofascial release, joint mobilization, spinal traction, rehab exercises, plus advanced options like decompression therapy, class-IV laser therapy, red-light therapy, and more.


TESTIMONIALS

"The Body Fix is your Chiropractic answer."
The Body Fix is your Chiropractic answer. I am more than willing to give this practice five stars. Having done the research and development to find these wonderful people, I can enthusiastically and honestly endorse this husband and wife team to anyone in the Mount Pleasant area in need of professional and courteous care. Do your self a favor and schedule one session so that you can enjoy a therapeutic and positive health experience. - Michael Dryden

"You’ll feel much better after a couple sessions"
If you’re looking for a chiropractor to fix all of your body aches and pains then look no further than The Body fix. Dr. Mario does an amazing job on the chiropractic and sports medicine therapy. Whether it’s your back or anywhere else, trust me when I tell you, you’ll feel much better after a couple sessions with him. The office also has laser therapy, a decompression table, and a vita light table. Maintaining a healthy body can be expensive, but the team here makes it worthwhile and you get your moneys worth by feeling healthy and restored.
- Matt Meisel

"He is one-of-a-kind"
Wow. I've been seeing chiropractors for about 30 years and have never encountered one like Dr Mario! He is intelligent, easy to talk to, a great listener, and cares very much about the health of his patients. But more than that he doesn't just adjust your spine and send you on your way. He spends about 30 minutes stretching and massaging muscles and decompressing the spine before he makes the adjustments. He is one-of-a-kind and I highly recommend!- Becca Bessinger

"The only ones that can get me back to 100%"
This place has changed my perspective on health care. They always excel above and beyond with my care and I can say every time I leave I’m feeling great and out of pain. I had back pain for years and I’m a golfer and they are the only ones that can get me back to 100%.- John Belicka
Our Trusted Partners




Get In Touch
Email: [email protected]
Phone Number:
843-981-4500
Clinic Hours
Mon – Thurs – 10:00am – 5:00pm
Friday – 9:00am – 1:00pm
Saturday & Sunday – CLOSED
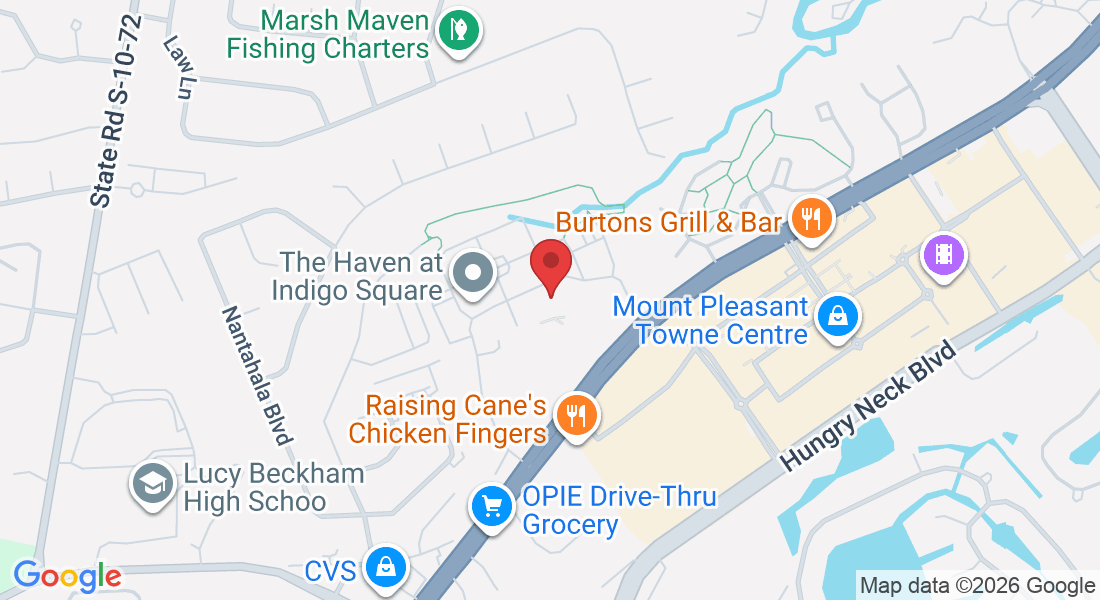
Address
1801 Indigo Market Drive, #205,
Mount Pleasant, SC, 29464
Tailored Care
Customized for real results.
Integrity
Honesty and transparency.
Excellence
Top-notch services.

Call
843-981-4500
Office:
1801 Indigo Market Drive, #205,
Mount Pleasant, SC, 29464
Email: [email protected]
FOLLOW US
TREATMENTS
CUSTOMER CARE
COMPANY
Copyright 2026. All Rights Reserved.